Why has a disease from the 1960s, considered eliminated, come back more than 60 years later?
Not even halfway through 2025, there are more than 700 cases confirmed in Texas alone, primarily in West Texas. Along with two confirmed deaths of unvaccinated children that had no underlying conditions, according to the Texas Department of State Health Services
The closest case to San Antonio is located in Atascosa County, 30 minutes from the Southside of the city.
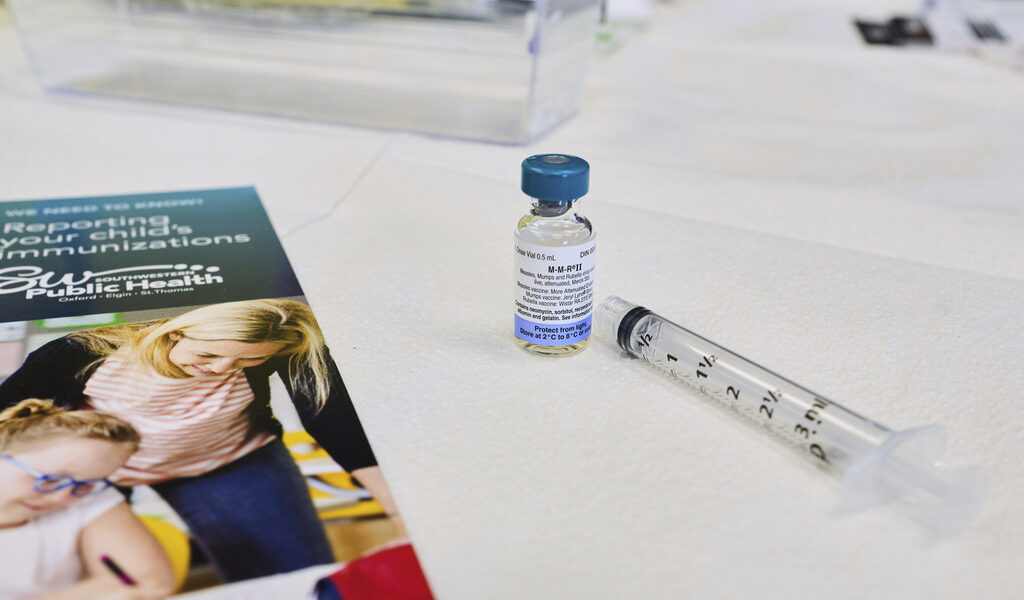
Bryan Bayles, an assistant professor of public health at Texas A&M University-San Antonio, says the main reason for the measles outbreak is the decline in the Measles, Mumps and Rubella vaccine rates. Gaines County is one of the areas where the MMR vaccine rate is lower than the 95% needed to maintain herd immunity and prevent outbreaks
Herd immunity refers to the percentage of the population that is vaccinated and how they “herd” and protect those close to them who are not vaccinated from getting exposed to the disease.
“Measles is extremely infectious, one of the most easily transmissible diseases,” Bayles said. “We need a high level of community vaccination so these outbreaks don’t spread beyond a few cases.”
Vaccine Hesitancy
Former physician Dr. Andrew Wakefield, who worked at the Royal Free Hospital in London as a gastroenterologist, claimed the MMR vaccine was linked to autism in 1998. Skepticism about vaccines grew after this event, causing a decline in vaccination rates.
This study was later debunked after various epidemiological trials, which are studies that examine how diseases spread and how effective treatments are.
“I’m a parent, I remember vaccinating my son and I empathize with that a hundred percent,” said Bayles about the hesitancy parents have of vaccinating their children. “But I also know the science, and I know that risk was much less likely than the risk of him getting a serious complication if he got measles.”
The first dose of the MMR vaccine was introduced in 1963 and the second recommended dose in 1989, with a success rate of 97% after both doses.
“Because [Measles] have been around so long, we’ve had a long time to observe them and the serious side effects from the vaccine [severe allergic reactions or seizures] are extremely rare,” Bayles said. “When you compare that to the risks of getting measles, it’s very stark.”
According to Bayles, about 30% of people infected with measles suffer from the most common complications, such as diarrhea, ear infections and pneumonia. In more serious cases, the virus can infect the brain and spinal cord which leads to brain swelling and death.
“What’s concerning is that there is a growing perception that the risks of vaccines are somehow greater than the risks of these illnesses,” Bayles said. “And the science shows that that’s simply not true.”
Should college students be concerned?
Age groups 5 to 17 years old continue to lead the majority of measles cases, but age groups 0 to 4 and 18 and older now follow close behind by a couple of cases.
According to Bayles, the reason why there is no longer a large gap in cases between age groups is because people between 20 to 30 years old who did not get vaccinated were kept from getting exposed due to the decent farm of herd immunity built in the late 90s and early 2000s.
Now, unvaccinated people 18 and older are being exposed by individuals and families who have been opting out of the MMR vaccine.
“If you know that you have been vaccinated, don’t worry,” Bayles said. “If you’ve gotten both doses, you’re pretty set, I wouldn’t sweat it at all.”
To learn more about what measles is, symptoms and where to find personal vaccine records, visit SA.gov/measles.
If students are interested in learning about effective communication in public health and risk-benefit profiles on vaccines, Bayles and Professor Monica Schoch-Spana will be teaching a Health Communication course in Spring 2026.